Spondylosis
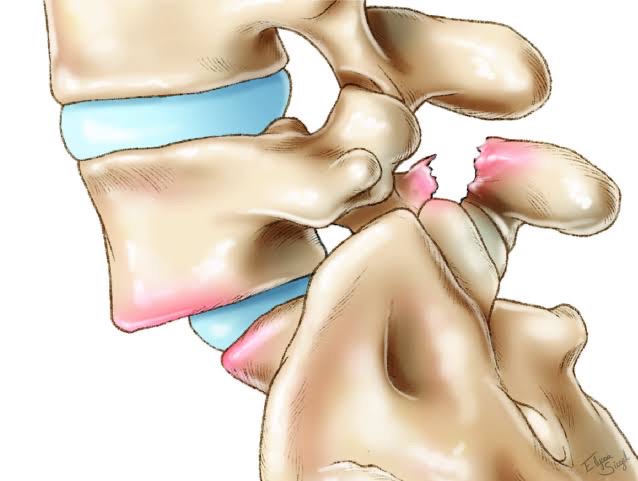
Spondylosis can affect any region of the spine. It is most common in the neck and lower back. It involves a defect in the pars interarticularis–a piece of bone attaching the facet joints at the back of the spine. This condition is a form of spinal degeneration occurring due to the natural effects of aging. As we grow older, normal wear and tear, as well as cellular changes, affect the structure of the spine. As a result, the soft tissues supporting the spine–discs, muscles, tendons, etc.–slowly begin to deteriorate. Spondylosis, however, doesn’t only affect older people. In fact, adolescents may develop the condition. Those participating in sports requiring repeated hyperextension of the lower back are at risk. This includes gymnastics, rowing, wrestling, and track & field sports. Younger people may not have many symptoms, so the condition may not get diagnosed. It spondylosis isn’t identified and managed correctly, however, it can result in more serious problems.
Diagnosing and Treating Spondylolysis
Young athletes and older adults suffering from lower back pain may want to get checked for spondylosis. One effective diagnostic test is the one-legged hyperextension Manoeuvre. While standing in a certain one-legged position, the lumbar spine gets stretched out. If this position causes pain it may indicate this condition. Also, X-rays, a bone scan, or MRI can help with diagnosis.
Treating spondylosis often involves conservative treatments like back braces, pain medications, and stretching exercises. If these treatments aren’t effective, surgery may be an option. Spinal decompression surgery or spinal fusion surgery can help relieve pressure on the affected area and provide much-needed stabilization.
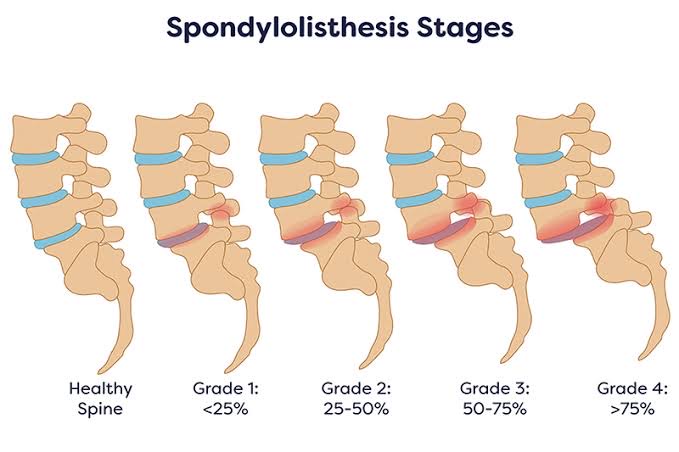
Spondylolisthesis
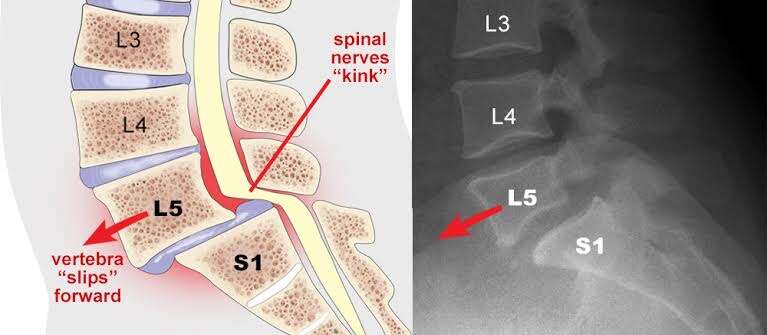
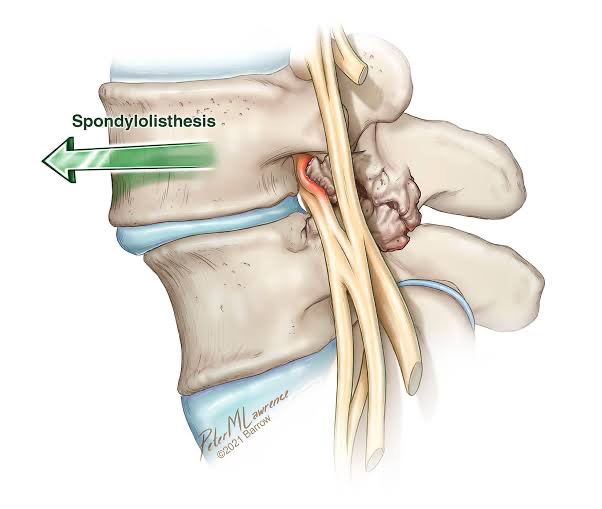
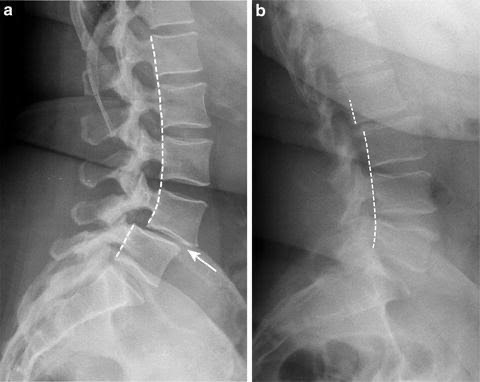
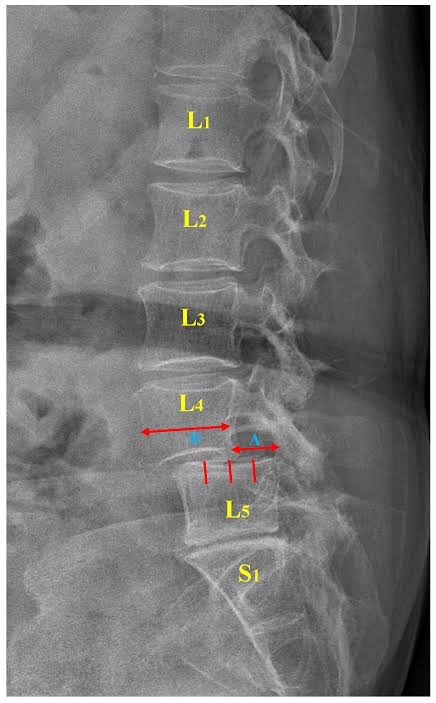
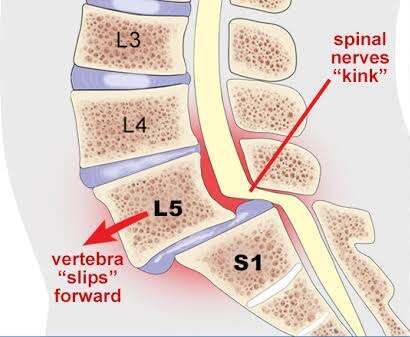
When spondylosis is left untreated, it may lead to Spondylolisthesis. Spondylosis involves the separation of the pars interarticularis. In contrast, spondylolisthesis is defined by a slipped vertebra. When one bone of the spine slips forward over another, it causes damage to the spinal structure. In some cases, a stress fracture may be to blame. Other times, damage to the intervertebral discs may cause this instability of the spine.
Family history and even congenital defects can contribute to this condition. It is often the result of certain sports and physical occupations. The lower back is responsible for carrying a lot of the body’s weight. Some activities make the spine more prone to developing spondylolisthesis. For example, gymnasts, football players, and weightlifters of all ages can develop this condition. Those that work in warehouses or delivering packages are also susceptible since they may bear a lot of weight on one side of the body and do a lot of bending. In addition, age-related degeneration of the spinal structures plays a role.
Some people don’t even know they have spondylolisthesis. They may discover it while getting an X-ray for an unrelated problem. Others experience low back pain, leg pain, swayback etc. Majority of the patients experience associated symptoms due to spinal canal stenosis.

Diagnosing and Treating Spondylolisthesis
If an X-ray suggests spondylolisthesis, your doctor may perform other tests or diagnostic imaging to get a better look at the problem. For example, your doctor may ask you to bend certain ways during an X-ray to see if your vertebrae are moving or unstable. MRI or CT Myelogram will help to see whether any nerve compression associated with spondylolisthesis.
During a physical exam, your doctor views your posture, range of motion, and overall physical condition. In addition, the doctor will test your reflexes as well as feeling for muscle spasms and abnormal curves in your spine. If you suffer from severe pain or haven’t responded to conservative treatments, surgery may be the next option. Spinal fusion surgery can be an effective treatment. Since it is a significant surgery, recovery times may be longer than other orthopedic procedures. By stabilizing the spine, however, it can prevent further structural damage and restore function and mobility. Depending on your condition and the surgeon’s preference, a lumbar interbody fusion .
0 Comments
* * * Get Free Bitcoin Now: https://modernpolytechnic.com/index.php?vwolg1 * * * hs=346c84ae0359af3774a8480ceb8167d1* ххх*
heuct5